Breaking Points: How OA and RA Challenge the Body in Different Ways
Kameron Hicks
Medical Affairs Intern
Arthritis encompasses a group of inflammatory conditions that affect the joints and surrounding tissues, leading to pain, swelling, and limited movement. The two most common forms are osteoarthritis (OA) and rheumatoid arthritis (RA).¹
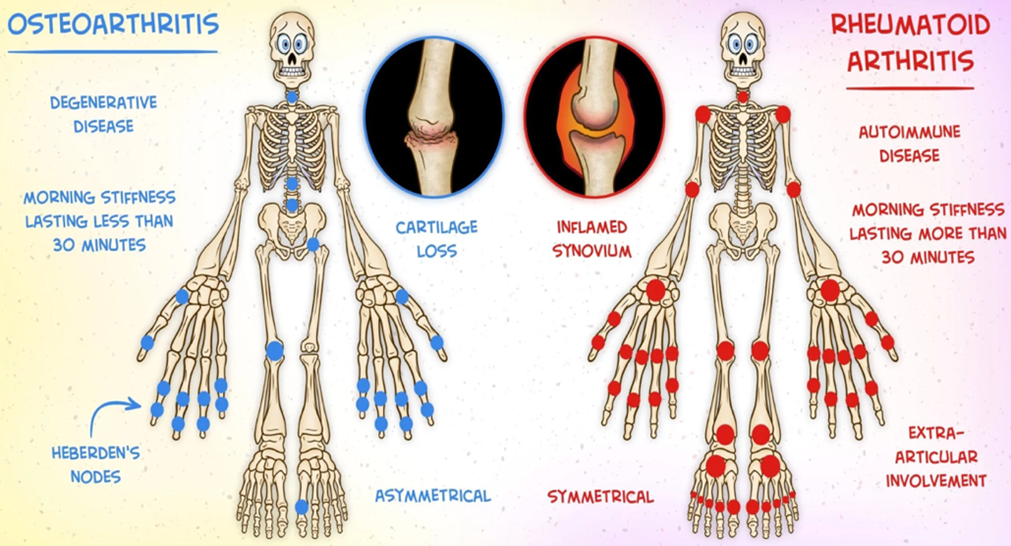
RA is an autoimmune disorder in which the body’s immune system attacks its own joint tissues, causing inflammation that leads to pain, stiffness, swelling, and redness, ultimately impairing joint mobility and function. Notably, RA symptoms often worsen after periods of rest and improve with activity as joint movement helps reduce inflammation and stiffness. The etiology of RA is believed to involve both genetic and environmental factors. Various alleles sharing a common amino acid sequence have been linked to RA development, and polymorphisms in other genes are associated with more severe disease. Cigarette smoking is the strongest environmental risk factor, while others include exposure to silica, asbestos, textile dust, and P. gingivalis. External antigens can trigger an autoimmune response that damages the joints.²
In contrast, osteoarthritis (OA) is a degenerative joint disease characterized by the progressive deterioration of articular cartilage. The loss of cartilage reduces cushioning and lubrication between bones, leading to friction, pain, stiffness, and decreased mobility. In contrast to RA, OA symptoms typically worsen with prolonged use and improve with rest, as mechanical stress aggravates joint pain. Pro-inflammatory mediators and proteolytic enzymes further contribute to joint destruction. As cartilage erosion progresses, chondrocytes proliferate and cluster, resulting in cartilage outgrowths and bone spurs. Continued damage to the collagen matrix triggers chondrocyte apoptosis, while abnormal collagen mineralization promotes subchondral bone thickening. Synovial inflammation and injury to surrounding joint structures, including ligaments, joint capsules, and menisci, may also occur.⁴
OA is classified as either primary or secondary. Primary OA develops with age in the absence of prior trauma or underlying disease, whereas secondary OA arises from joint abnormalities or injury. Major risk factors include advanced age, female sex, obesity, and a history of joint injury.⁵
Both OA and RA are characterized by joint pain, swelling, and reduced mobility. Although their specific causes are not fully understood, a combination of genetic, environmental, and lifestyle factors contributes to their development.
References:
- Johns Hopkins Medicine. Arthritis. Updated February 2025. Accessed October 14, 2025. https://www.hopkinsmedicine.org/health/conditions-and-diseases/arthritis
- American College of Rheumatology. Rheumatoid Arthritis. Updated February 2025. Accessed October 14, 2025. https://rheumatology.org/patients/rheumatoid-arthritis
- Chauhan K, Jandu JS, Brent LH, et al. Rheumatoid Arthritis. [Updated 2023 May 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK441999/
- Cleveland Clinic. Osteoarthritis: Symptoms, Causes & Treatment Options. Updated October 2, 2023. Accessed October 14, 2025. https://my.clevelandclinic.org/health/diseases/5599-osteoarthritis
- Sen R, Hurley JA. Osteoarthritis. [Updated 2023 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK482326/
- Osteoarthritis vs. Rheumatoid Arthritis. MedComic. Accessed October 14, 2025. https://www.medcomic.com/medcomic/osteoarthritis-vs-rheumatoid-arthritis
The information provided is for general informational and educational purposes only. It is not intended to serve as medical advice, diagnosis, or treatment. The content is written by a licensed pharmacist and reflects general knowledge and expertise in the healthcare field, but it is not a substitute for professional medical advice from a qualified healthcare provider.
Always consult your physician, pharmacist, or other qualified healthcare professional before starting, stopping, or modifying any medication, treatment, or health regimen. Individual health conditions and needs vary, and only a healthcare professional can provide personalized advice tailored to your specific situation.
While we strive to ensure the accuracy and currency of the information presented, medical knowledge is constantly evolving, and errors or omissions may occur. The blog’s content does not cover all possible uses, precautions, side effects, or interactions of medications or treatments. Reliance on any information provided is solely at your own risk.
Links to external websites or resources are provided for convenience and do not imply endorsement or responsibility for their content.






